Resources
Mediators of Wound Healing: Cytokines, Growth Factors, and Inflammatory Control
The human body is remarkably adept at repairing itself, both from injuries and infections, and inflammation is an essential part of that process. Activating and controlling the immune response involves many signaling molecules, particularly pro-inflammatory cytokines and anti-inflammatory growth factors. Gaining a better understanding of cytokines and growth factors is essential to developing targeted therapies, optimizing surgical site and wound healing, and advancing regenerative medicine.
“By targeting the factors that can lead to chronic wounds, such as co-morbidities like diabetes, blood pressure, smoking, and the presence of microbes, whether infectious or commensal, we can create complex medical products that work to reduce microbial load and the chance for biofilms and infections. These devices may impact the cytokine profile of the wound or surgical site and ultimately help patients by reducing their healing time,” said Greg Mouchka, President of iFyber.
The Stages of Wound Healing
Cytokines or growth factors play critical roles in every phase of healing. There are four stages of wound healing, and while each is distinct, they also overlap.
The first phase, hemostasis, is an immediate response to injury that involves clot formation and vasoconstriction. Early inflammatory cytokines help initiate this process and trigger platelet activation and the release of pro-inflammatory mediators, preparing the body for the next phase.
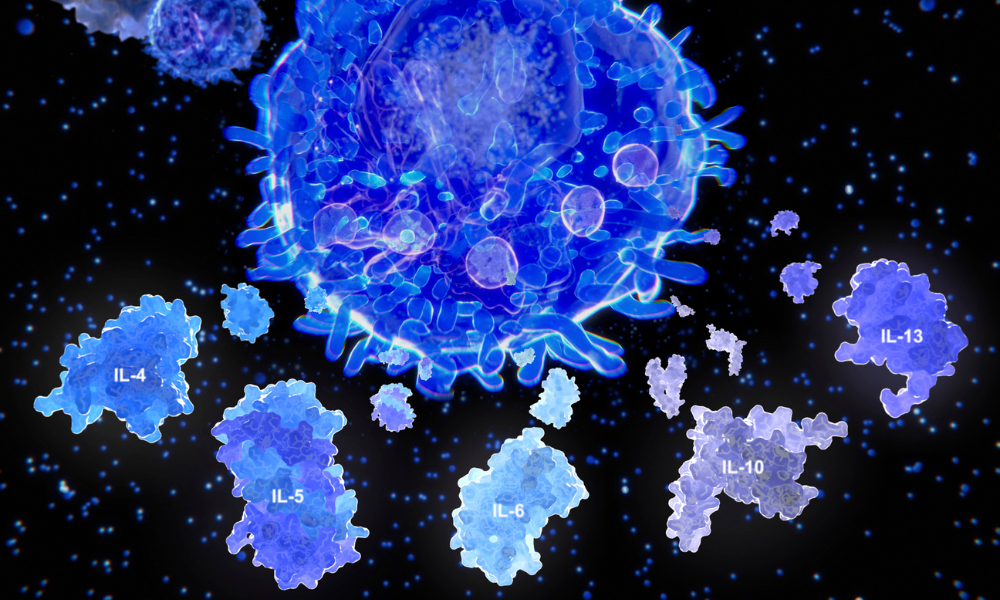
The inflammatory stage soon begins and can last for several days. Cytokines are heavily involved in this phase. Pro-inflammatory cytokines activate the NF-κB signaling pathway, which leads to the production of additional pro-inflammatory cytokines that sustain the immune response and drive wound healing.
The next stage is proliferation, during which the wound begins to rebuild through fibroblast migration, angiogenesis, and tissue formation. Growth factors play significant roles in this phase by activating pathways to promote cell proliferation and migration for wound closure and tissue repair.
The final stage, known as remodeling or maturation, involves the reorganization and strengthening of the extracellular matrix. This process typically begins a few weeks after injury and can continue for months or even years, depending on the severity of the wound. Growth factors play a crucial role in orchestrating this phase by regulating fibroblast activity, extracellular matrix remodeling, and scar formation.
Inflammation Stimulation: Pro-Inflammatory Cytokines
TNF-α (Tumor Necrosis Factor-alpha)
TNF-α is a potent pro-inflammatory cytokine. Prominent during the inflammatory phase, it promotes immune cell recruitment and enhances vascular permeability. However, overexpression of TNF-α can lead to chronic wounds and fibrosis. TNF-α is also overactive in conditions like rheumatoid arthritis, psoriasis, and inflammatory bowel disease.
Clinically, TNF-α is targeted in autoimmune diseases with anti-TNF biologics, such as infliximab and adalimumab. Research continues to explore whether TNF-α inhibition in chronic non-healing wounds can promote better outcomes and reduce excessive inflammation.
IL-6 (Interleukin-6)
IL-6 plays a dual role in wound healing by promoting immune cell recruitment in the early inflammation phase while also aiding the transition to tissue repair. IL-6 is a key driver of inflammation in inflammatory diseases and cytokine storm syndromes. Also, its levels in post-surgical recovery may serve as predictors of healing efficiency.
Monitoring IL-6 in post-surgical patients can help guide interventions, such as anti-inflammatory therapies or regenerative treatments. Research into IL-6 inhibitors is ongoing to better control its effects in chronic wounds and systemic inflammatory diseases.
IL-1β (Interleukin-1 Beta)
In wound healing, IL-1β drives the early inflammatory response by increasing neutrophil infiltration, which are among the first immune cells to arrive at the wound site. However, when unregulated, IL-1β is linked to chronic wounds and excessive scarring.
IL-1β is a potential biomarker for predicting delayed wound healing. Research is examining ways to regulate its levels to enhance tissue repair while minimizing excessive inflammation.
“One of the services we provide to medical device manufacturers is evaluating the levels of cytokines in in vitro models of healing. These sandwich-based assay arrays allow us to evaluate dozens of cytokines in a semiquantitative fashion. By comparing to a control, this gives us a vision into how a device influences the wound healing process by moderating cytokine prevalence. For example, we may monitor a device that reduces TNF-α to discover if it has an impact on healing chronic wounds,” said Mouchka.
Healing Agents: Anti-Inflammatory Growth Factors
TGF-β (Transforming Growth Factor-beta)
TGF-β is essential for proper tissue regeneration, regulating fibroblast activation and extracellular matrix production. However, excessive TGF-β signaling can lead to fibrosis.
Clinically, TGF-β modulation is targeted in fibrosis therapy and regenerative medicine, particularly in conditions involving excessive scarring or deficient healing. Understanding TGF-β regulation is crucial for developing precision medicine strategies in wound healing, organ repair, and tissue engineering while mitigating its profibrotic effects.
EGF (Epidermal Growth Factor)
EGF stimulates keratinocyte proliferation and migration, the primary cell type found in the epidermis. EGF is crucial in the proliferation stage of wound healing, promoting regeneration of the epidermis.
EGF-based therapies are used in burn treatments, chronic wound healing, and regenerative medicine to accelerate skin repair. Research is exploring bioengineered EGF delivery systems (such as topical gels, nanoparticles, and skin grafts) for enhanced wound recovery.
VEGF (Vascular Endothelial Growth Factor)
VEGF plays an essential role in the proliferation stage of wound healing by promoting new blood vessel formation. VEGF activates signaling pathways that stimulate endothelial cell proliferation, migration, and differentiation.
VEGF is a target in therapies for chronic wounds, diabetic ulcers, and ischemic conditions, where inadequate blood supply hinders healing. It is also modulated in cancer treatments to limit tumor vascularization. Researchers are investigating VEGF-based therapies, including bioengineered scaffolds, gene therapy, and VEGF-mimicking drugs, to optimize wound healing and tissue regeneration.
iFyber is an Experienced CRO Partner for Wound Healing Innovations
“Organizations that are researching and developing engineered solutions to growth factor delivery need a partner that fully understands the cell and tissue culture environment and can perform the assays that can quantify the growth factors,” said Mouchka. “iFyber can assist in the formulation, delivery, and verification of results as part of the growth-factor-delivery development process. We can also evaluate a device’s ability to promote the formation of growth factors in living human-skin-equivalent models of healing.”
Whether you’re exploring new treatments for chronic wounds, optimizing post-surgical recovery, or advancing biomaterial innovation, iFyber can provide the scientific expertise, technical support, and cutting-edge solutions needed to accelerate your research and product development. Connect with iFyber today to learn how partnering with iFyber can bring your innovations to life.
