Resources
The Role of Human Skin Equivalent (HSE) Models in Advancing Monoclonal Antibody Drug Development
Monoclonal antibody (mAb) drug development is rapidly evolving, driven by growing demand for precision therapies and a regulatory push toward non-animal testing methods. In this dynamic environment, Human Skin Equivalent (HSE) models are emerging as a powerful preclinical tool, especially for mAbs targeting dermatologic conditions or systemic diseases with skin involvement.
As the FDA moves to phase out mandatory animal testing for certain therapeutics, including biologics like monoclonal antibodies, HSEs offer a human-relevant alternative for early-stage evaluation. These models are more than just ethical stand-ins for animal use—they provide a mechanistic, translational bridge that enhances our ability to understand, optimize, and de-risk antibody-based therapeutics.
Let’s explore how HSEs are reshaping how scientists develop and refine monoclonal antibodies.
Human Skin Equivalent Models and mAb Drug Development
Mechanistic Insights and Target Validation
In drug discovery, understanding the underlying biology is half the battle. HSE models offer a controlled, reproducible, and human-relevant environment to study skin pathophysiology and validate drug targets.
For monoclonal antibodies targeting specific immune molecules, such as cytokines or immune checkpoints, HSEs provide the structural and cellular complexity needed to evaluate how those targets behave in actual human skin. Conditions like psoriasis, atopic dermatitis, or cutaneous lupus often involve intricate crosstalk between immune cells and skin cells. HSEs can replicate these interactions more effectively than animal models, which often lack the necessary human-specific molecular context.
By mimicking disease states within a human-derived matrix, researchers can more accurately assess whether a proposed mAb target is not only present, but therapeutically actionable in a clinical context.
Functional Testing of Antibody Efficacy
Once a target is validated, researchers need to understand how effectively a monoclonal antibody can inhibit or modulate that target. Human skin equivalents provide flexible platforms for both localized and systemic-like delivery of therapeutic antibodies, allowing scientists to evaluate:
- Direct topical application: Assess local pharmacodynamics and target engagement when antibodies are applied to the skin model, allowing researchers to observe how the antibody diffuses through the epidermal layers and interacts with target proteins.
- Systemic delivery mimicry: HSEs can be co-cultured with immune cells such as T cells or macrophages, creating a microenvironment that approximates immune trafficking and activation, allowing researchers to monitor not just antibody binding, but also downstream effects like cytokine suppression or signaling pathway inhibition
- Biomarker tracking: Quantitative readouts, including changes in cytokine levels, gene expression profiles, and histological markers, help create a comprehensive picture of therapeutic efficacy before moving into animal or human trials.
Modeling Inflammatory Skin Diseases
One of the most powerful uses of HSEs is their adaptability to simulate disease states. Incorporating specific cytokines or environmental triggers enables researchers to induce skin inflammation that mimics clinical conditions.
For instance, adding TNF-α and IL-17 to the skin model can induce the epidermal hyperplasia and immune activation seen in psoriasis. Similarly, IL-4 and IL-13 can be used to model the immune-skewing and barrier dysfunction associated with atopic dermatitis. Even external triggers, such as ultraviolet radiation or contact allergens, can be layered into these models to simulate flares or acute exacerbations.
With a disease model in place, researchers can then introduce candidate monoclonal antibodies—like secukinumab (anti–IL-17A) or adalimumab (anti–TNF-α)—and assess their ability to reverse or modulate the inflammatory cascade. This not only improves confidence in clinical efficacy but also helps fine-tune dosing and delivery strategies.
Simulating Human Immune Interactions
Modern monoclonal antibodies do more than block pathways—they actively shape immune responses. That’s why it’s increasingly important to study how these therapies interact with immune cells in a human-specific environment.
Advanced HSE models incorporate a range of immune cells, such as dendritic cells, macrophages, and T cells, to better reflect the immunological complexity of human skin. These models allow researchers to explore interactions such as Fc receptor binding, antibody-dependent cellular cytotoxicity (ADCC), and cytokine release in response to antibody treatment.
For immunotherapies and checkpoint inhibitors, these insights are essential. They help determine whether the antibody is activating or suppressing immune responses appropriately, and whether it might trigger unintended immune activation—a key safety concern in early-stage development.
Safety and Toxicology Screening
Even the most targeted biologics carry the potential for off-target effects or immunogenicity. Traditional safety testing often relies on animal models that poorly replicate human skin response, whereas human skin equivalents offer a valuable early-stage screening platform for evaluating local toxicity and tolerability.
Researchers can utilize HSEs to monitor for:
- Tissue irritation and sensitization
- Barrier disruption
- Immune-mediated inflammation
- Histopathological evaluation of tissue damage
- Assessment of dose-dependent toxicity
- Early signs of allergic or autoimmune responses
Because HSEs are derived from human cells and replicate human skin architecture, they provide a more predictive assessment of tolerability than rodent skin or 2D cultures. This proactive approach not only supports regulatory compliance but can flag liabilities before advancing to costly clinical trials, reducing the risk of trial failure and improving patient safety.
3D Vs 2D Models: Physiological Relevance Matters
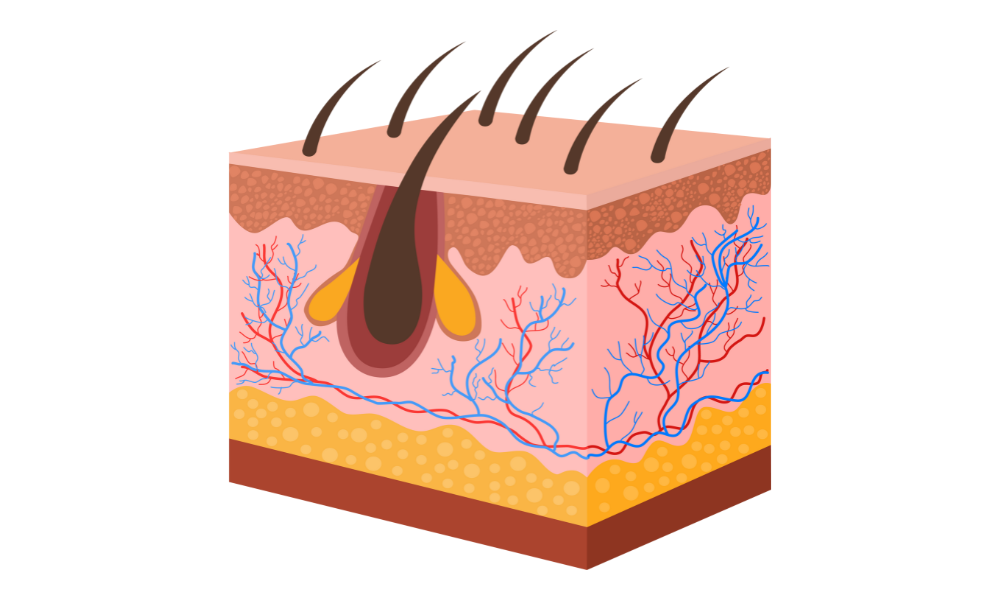
At the core of the HSE advantage is its three-dimensional structure, which closely mimics real human skin. Unlike traditional 2D cultures of keratinocytes or fibroblasts, HSEs recreate the stratified architecture of the epidermis and dermis, including critical features like:
- Barrier function, which impacts drug absorption and retention
- Dermal-epidermal interactions, crucial for inflammation and repair signaling
- Metabolic activity, which influences antibody stability and efficacy
This level of physiological relevance translates to more accurate predictions of pharmacokinetics and pharmacodynamics. For researchers, it means fewer surprises in downstream animal or clinical testing—and a faster path to therapeutic validation.
Human Skin Equivalent Models Offer A New Paradigm for mAb Innovation
As regulatory agencies embrace non-animal approaches and the pharmaceutical industry seeks more predictive, human-centric tools, Human Skin Equivalent models represent a critical innovation. These models offer a unique intersection of biological relevance, experimental control, and clinical translatability, enabling scientists to interrogate complex mechanisms, evaluate efficacy, and screen for safety in a way that aligns with human biology and clinical relevance.
At iFyber, we’re excited by how these models can shift how biologic development is approached. Whether you’re advancing a novel immunotherapy or refining an existing antibody platform, human skin equivalent models offer a smarter path forward.
Ready to bring HSEs into your monoclonal antibody development program? Contact iFyber to learn how our in vitro models and preclinical R&D services can support your innovation pipeline.
Download our white paper, 3D Human Epidermis Equivalent (HEE) Model And Its Applications, for more information on our models.
